SITE OF INFECTION, PATHOLOGY AND DISEASE SYMPTOMS
Candida albicans (C. albicans) usually affects mucosal surfaces such as the vagina, mouth, intestinal tract, or skin folds where moisture collects. This yeast normally lives harmlessly in these areas, but when the natural balance of bacteria and yeast changes, it begins to multiply. C. albicans can switch to its hyphae form, attach to epithelial cells, and begin invading the tissue.
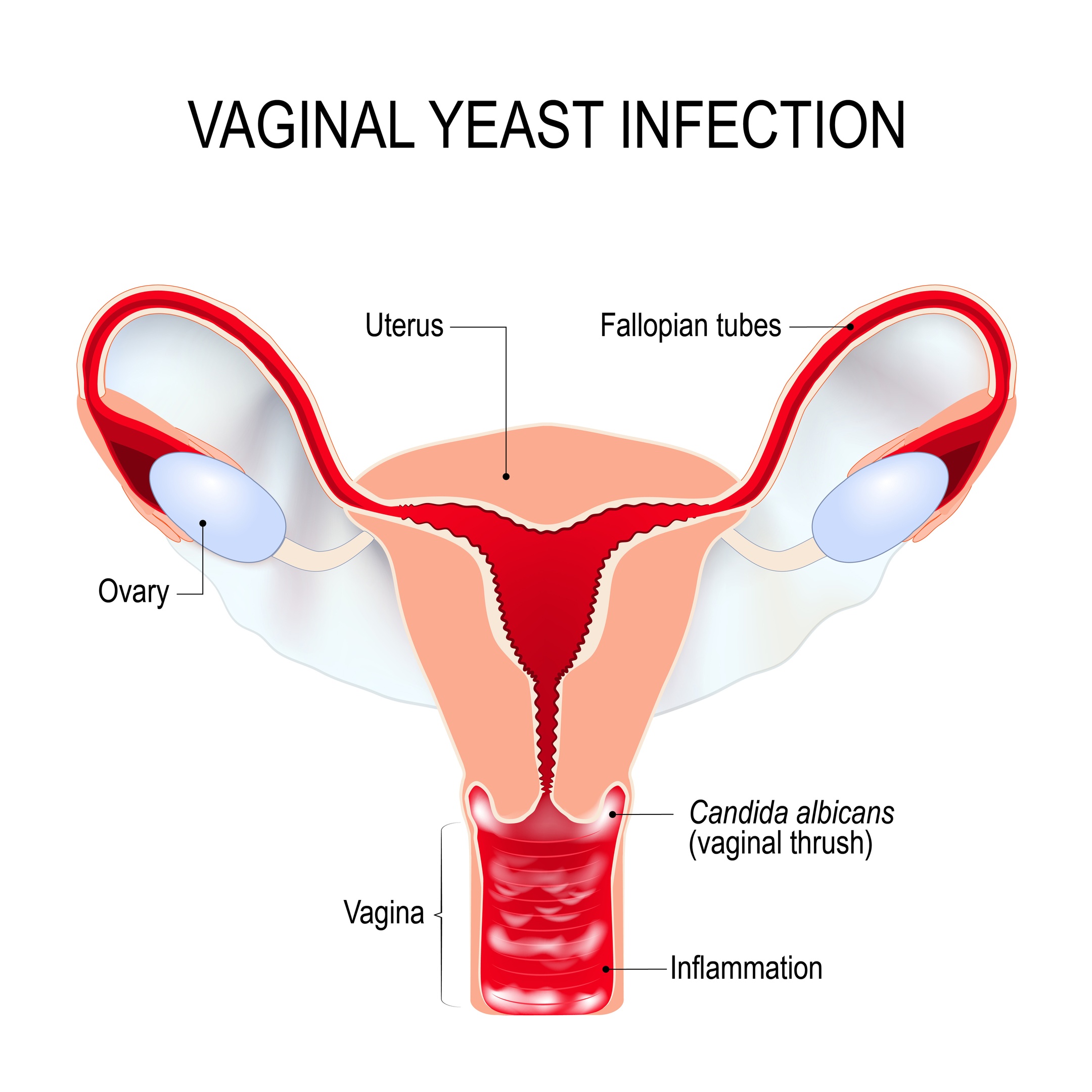
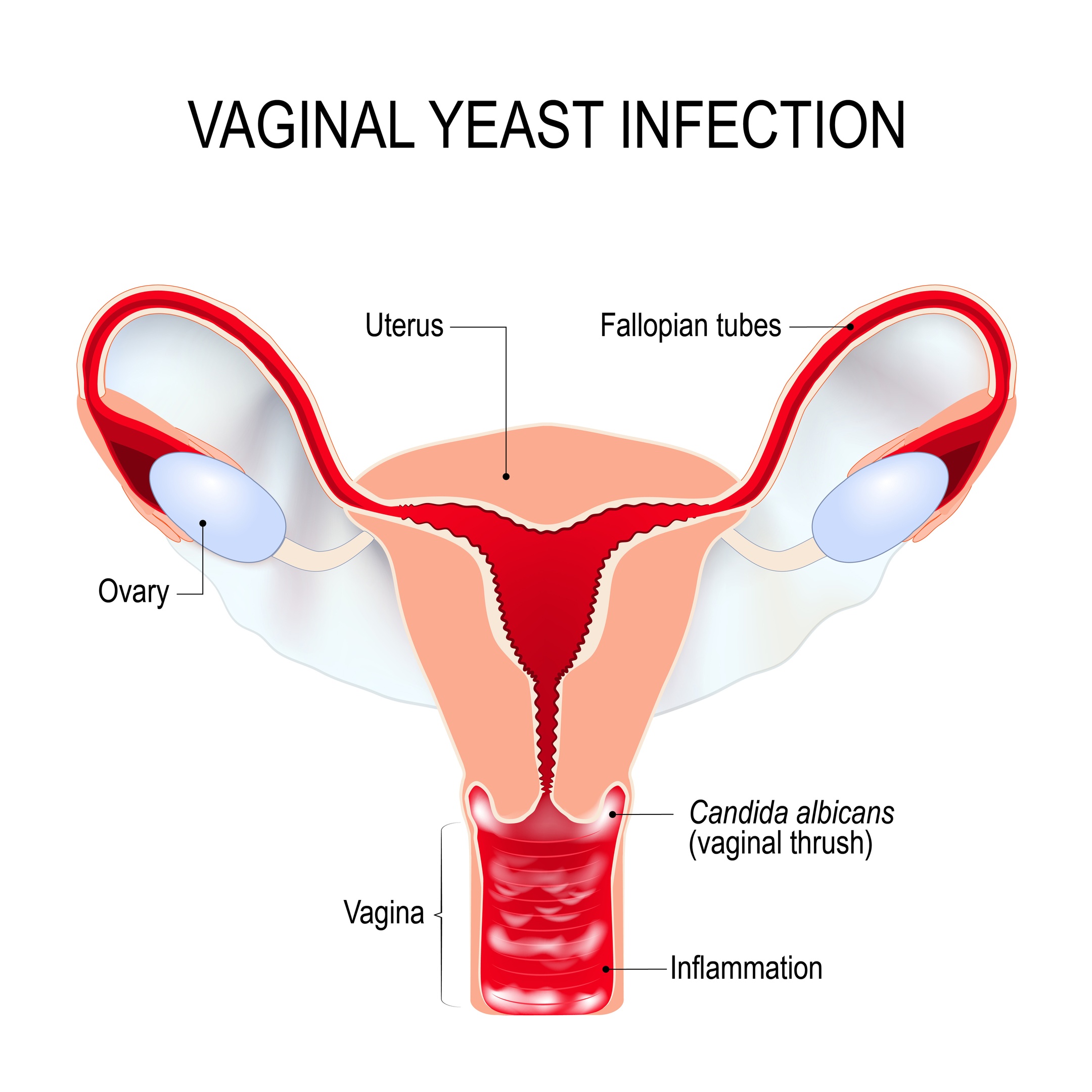
As the yeast grows in and spreads, it irritates the surrounding tissues, which triggers an inflammatory response. This inflammation causes redness, swelling, itching, and irritation. In vaginal infections, thick white discharge often appears because the yeast and immune cells mix with shed epithelial cells. Some people also experience pain during urination or intercourse. On the skin, the infection causes a red, itchy rash, often in warm and moist areas like under the breasts, in the groin region, or between skin folds.
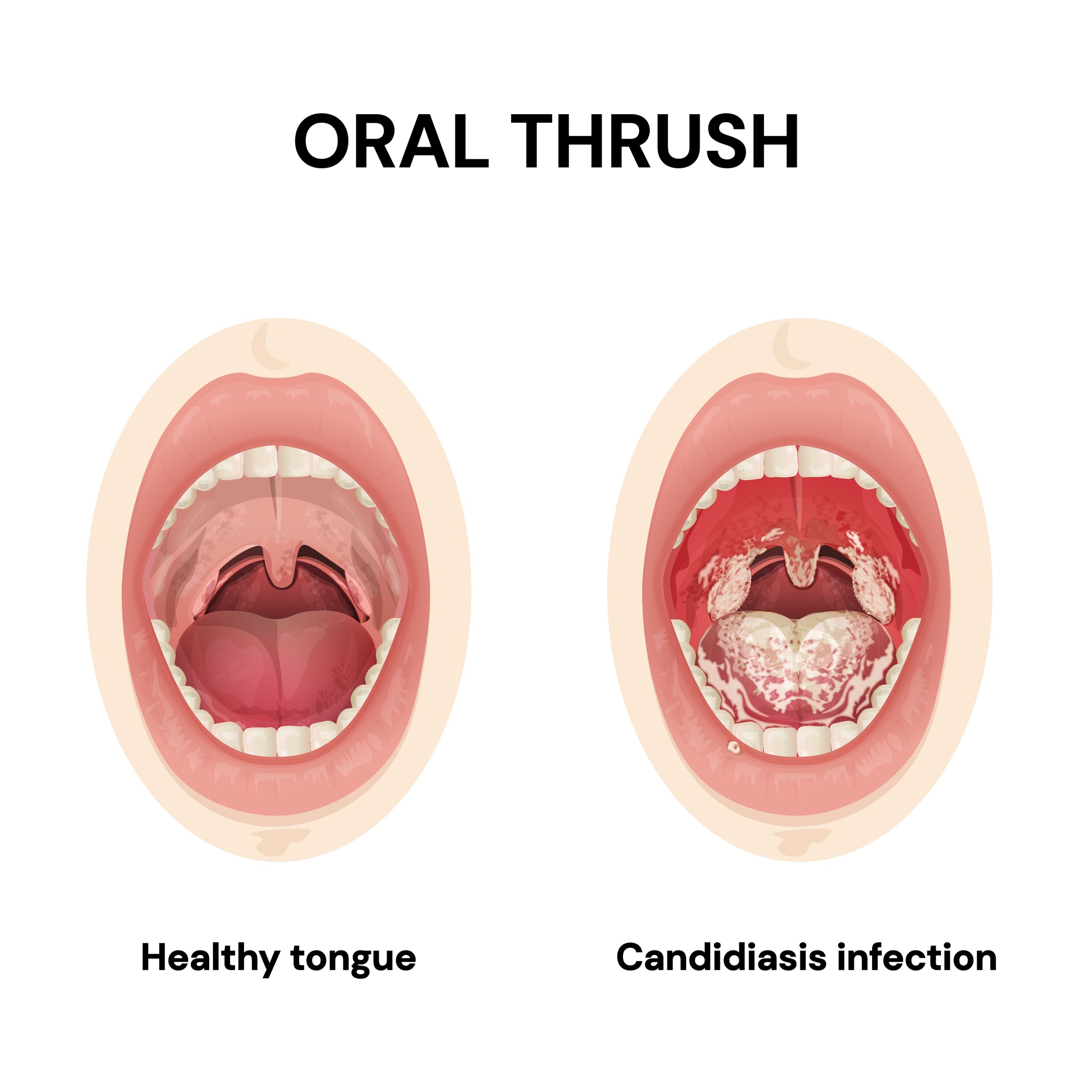
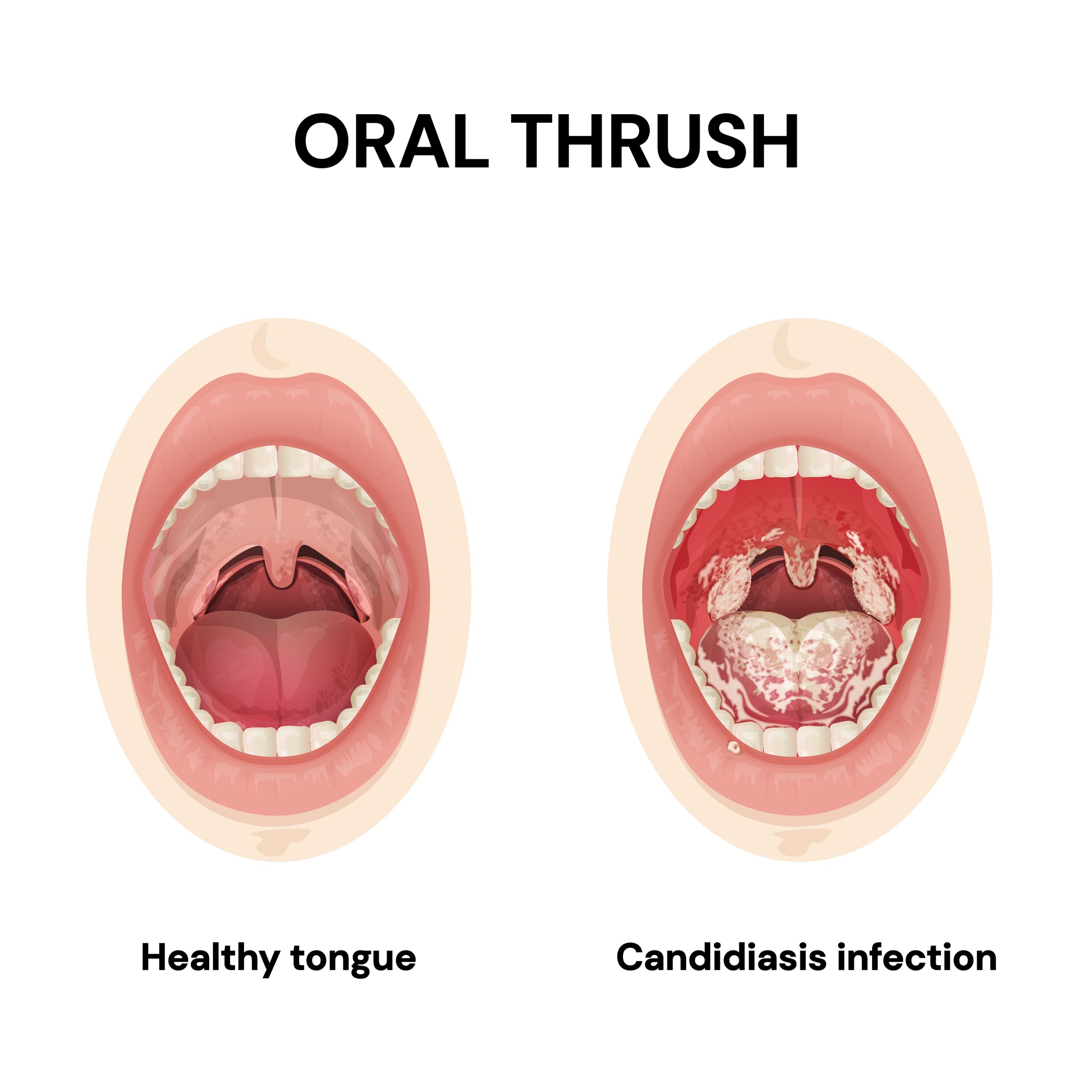
In the mouth, infection is known as oral thrush, which causes white, creamy patches on the tongue, inner cheeks, and roof of the mouth. These patches may be painful and can bleed slightly if scraped. Symptoms can also include soreness, difficulty swallowing, or a burning feeling in the mouth.
The immune system really plays an important role when it comes to controlling C. albicans. When a person’s immunity is weakened, such as during an illness or chemotherapy, the fungus can be spread more easily and become much more serious. In rare and serious cases, like particularly in hospitalized or immunocompromised patients, C. albicans can enter through the bloodstream and spread to organs such as the kidneys, heart, or liver. This condition is called invasive candidiasis and it can cause fever, chills, and some serious complications which needs immediate medical treatment.
Overall, C. albicans causes disease by attaching to tissues, invading the surface cells, and triggering inflammation. While most of the infections stays on the skin or mucous membranes and are uncomfortable rather than being dangerous, the fungus can become life-threatening if it spreads deeper in people with weakened immune defences.